Signs and symptoms
Common symptoms can include:
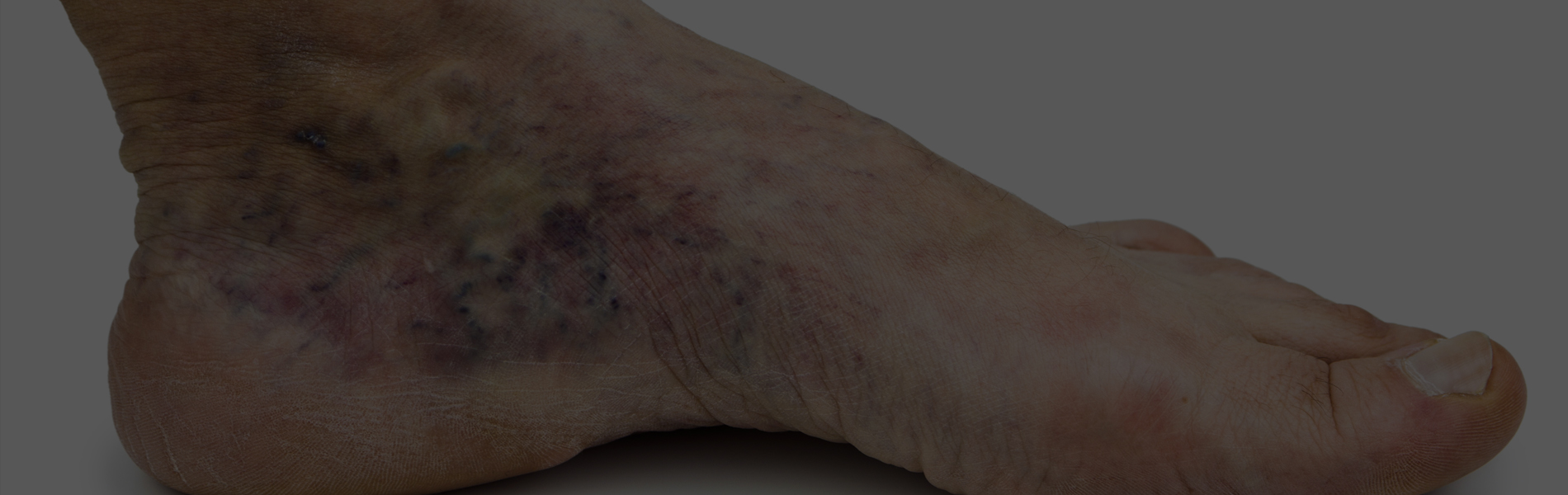
- Bulging or twisting of the affected vein(s)
- Aching of the affected area, especially after sitting or standing for lengthy periods
- Swelling in the legs
- A feeling of heaviness and muscle fatigue in the legs
- Itching around the affected veins
- Leg cramps at rest
Causes
A number of factors contribute to the development of varicose veins. These include:
- A genetic predisposition to develop varicose veins
- Hormonal factors
- Excess weight
- Pregnancy
- Circulatory problems, such as blood clots (thrombosis)
- Injury or inflammation of the veins
- Chronic constipation may contribute to the development of rectal varicose veins (haemorrhoids)
SURGICAL TREATMENT
If the vein junction where the varicose vein originates has been shown by an ultrasound scan to be incompetent (allowing blood to flow backward), then the most common surgical treatment is to tie off the varicose vein at this junction. Surgery involves making a small incision in the leg, locating the vein junction and tying off the varicosed vein. The vein is left in place, however blood is prevented from flowing into it. Another common surgical technique for treating superficial varicose veins is “vein stripping” – where the affected vein is completely removed.
Both types of surgery can be performed under general or spinal anaesthetic and a stay in hospital may be required. At the completion of surgery, the incisions in the skin are closed with small stitches to minimise scarring. Bandages or elasticised stockings are then applied to gently compress and support the leg and to reduce swelling. These may need to be worn for up to six weeks, the stitches are usually removed seven – 10 days after surgery.